Is the use of intraoperative heparin safe?
The use of intraoperative heparin is a medical decision that depends on various factors, including the specific surgical procedure, the patient's medical history, and the risks and benefits associated with anticoagulation therapy. Intraoperative heparin is often administered to prevent blood clot formation during certain surgical procedures, particularly those involving blood vessels or the heart.
Here are some considerations regarding the safety of intraoperative heparin usage:
Surgical Procedures:
- Intraoperative heparin is commonly used during surgeries such as cardiac bypass surgery, vascular surgery, and other procedures where preventing blood clot formation is crucial.
Anticoagulation Therapy:
- Heparin is an anticoagulant, meaning it helps prevent the formation of blood clots. The use of heparin during surgery is carefully managed to balance the need for anticoagulation with the risk of bleeding.
Risk of Thrombosis:
- In certain surgeries, there is an increased risk of thrombosis (formation of blood clots). In these cases, heparin may be administered to reduce the risk and improve the overall safety of the procedure.
Individual Patient Factors:
- The decision to use intraoperative heparin is based on the individual patient's medical history, including their risk factors for clotting or bleeding. The patient's overall health, medications, and coexisting conditions are taken into consideration.
Monitoring:
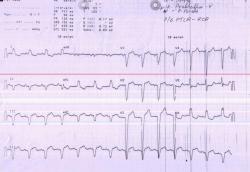
- Intraoperative heparin usage is closely monitored to ensure that the patient's blood remains within a safe anticoagulation range. Coagulation tests, such as activated clotting time (ACT) or activated partial thromboplastin time (aPTT), may be used to monitor the anticoagulant effect.
Reversal Agents:
- In the event of excessive anticoagulation or bleeding complications, reversal agents such as protamine sulfate may be administered to counteract the effects of heparin.
Collaboration Between Surgical and Anesthesia Teams:
- The decision to use intraoperative heparin is often a collaborative effort between the surgical and anesthesia teams. The teams work together to assess the patient's risk factors and determine the appropriate anticoagulation strategy.
It's important to note that the safety of intraoperative heparin usage is context-specific and should be determined by the patient's healthcare team based on individual circumstances. Healthcare professionals carefully weigh the potential benefits of preventing clot formation against the risks of bleeding, taking into account the specific surgical context and the patient's overall health.
Patients should discuss any concerns or questions about their treatment plan, including the use of heparin, with their healthcare providers.
Assessing the risks and benefits of using intraoperative heparin
Benefits
Reduced risk of thromboembolic complications: Intraoperative heparin can help prevent blood clots from forming during surgery, especially in patients at high risk of thrombosis.
Improved graft patency: In certain procedures, such as vascular surgery, intraoperative heparin can promote graft patency and reduce the risk of graft failure.
Decreased mortality: Studies have shown that intraoperative heparin may be associated with reduced mortality in certain surgical procedures.
Risks
Bleeding: The most significant risk of intraoperative heparin is bleeding. This risk is increased in patients with coagulopathies, thrombocytopenia, or other conditions that affect blood clotting.
Heparin-induced thrombocytopenia (HIT): HIT is a rare but serious complication that can occur with heparin administration. HIT can lead to thrombosis and severe bleeding.
Allergic reactions: Heparin can cause allergic reactions, ranging from mild skin rash to anaphylaxis.
Indications for intraoperative heparin administration
Intraoperative heparin is typically considered for patients at high risk of thromboembolic complications, such as those with:
Venous thromboembolism (VTE): History of VTE, active VTE, or risk factors for VTE
Major vascular surgery: Surgery involving major blood vessels, such as aortic aneurysm repair or coronary artery bypass grafting (CABG)
Certain orthopedic procedures: Total hip or knee arthroplasty
Contraindications and precautions for intraoperative heparin use
Intraoperative heparin is contraindicated in patients with:
Active bleeding or recent major bleeding episode
Severe coagulopathy or uncontrolled bleeding disorder
Severe heparin allergy or documented HIT
Patients receiving thrombolytic therapy
Precautions should be taken in patients with:
Renal impairment: Heparin clearance may be reduced in patients with renal impairment, increasing the risk of bleeding.
Hepatic impairment: Heparin metabolism may be altered in patients with hepatic impairment, affecting heparin levels and bleeding risk.
Pregnancy: Heparin use in pregnancy should be carefully considered and balanced against potential risks to the fetus.
Monitoring strategies to ensure patient safety during intraoperative heparin administration
Close monitoring is crucial during and after intraoperative heparin administration to ensure patient safety and minimize bleeding complications.
Platelet count: Regular monitoring of platelet count is essential to detect and manage any heparin-induced thrombocytopenia (HIT).
Activated coagulation time (ACT): ACT monitoring helps assess heparin's anticoagulant effect and guide heparin dosage adjustments.
Bleeding assessment: Continuous observation of the surgical site and monitoring of vital signs are crucial to detect early signs of bleeding.
Postoperative monitoring: Platelet count and ACT monitoring should continue in the postoperative period, especially in high-risk patients.
Minimizing complications and optimizing patient outcomes with intraoperative heparin
Individualized heparin dosing: Heparin dosage should be tailored to the patient's weight, underlying conditions, and potential bleeding risk.
Careful patient selection: Patients should be carefully evaluated for potential risks and benefits of intraoperative heparin based on their individual risk factors.
Prompt reversal of heparin: Reversal agents, such as protamine sulfate, should be readily available to promptly reverse heparin's anticoagulant effect in case of excessive bleeding.
Effective communication and collaboration: Clear communication and collaboration between the surgical team, anesthesia team, and hematology team are essential for safe and effective heparin administration.