How do you titrate heparin drip?
Titration of a heparin drip involves adjusting the dosage to maintain a targeted level of anticoagulation, as measured by parameters such as the activated partial thromboplastin time (aPTT) or activated clotting time (ACT). The goal is to prevent excessive clotting without causing bleeding complications. It's important to note that the procedure for titrating heparin should be carried out by qualified healthcare professionals, and the information provided here is for general knowledge purposes only.
Here are general steps involved in titrating a heparin drip:
Baseline Assessment:
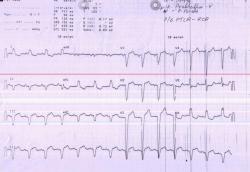
- Before initiating heparin therapy, assess the patient's baseline coagulation status, including aPTT or ACT values.
Initiate Heparin Infusion:
- Start the heparin infusion at the prescribed initial rate as per the medical order.
Frequent Monitoring:
- Monitor coagulation parameters regularly, typically every 6 hours or as specified by the healthcare provider. The primary goal is to maintain the aPTT within a therapeutic range.
Adjustment Criteria:
- The decision to titrate heparin is based on the aPTT or ACT values. If the values are below the therapeutic range, the heparin infusion rate may be increased. If values are above the therapeutic range, the rate may be decreased.
Dose Adjustment:
- Adjust the heparin infusion rate according to a predetermined protocol or based on the healthcare provider's order. The adjustment may involve increasing or decreasing the infusion rate by a specified amount or percentage.
Reassessment:
- Reassess coagulation parameters after each dose adjustment to ensure that the desired therapeutic range is achieved.
Documentation:
- Document the heparin infusion rate, coagulation parameters, and any adjustments made in the patient's medical record. Accurate documentation is crucial for tracking the patient's response to therapy.
Frequent Patient Assessment:
- Monitor the patient for signs of bleeding or other adverse effects. Assess vital signs regularly, and be alert to any changes in the patient's condition.
Collaboration with Healthcare Team:
- Communicate with the healthcare team, including physicians, nurses, and pharmacists, to discuss the patient's response to heparin therapy and to make informed decisions about dose adjustments.
Review and Repeat:
- Continuously review the patient's response to heparin therapy and adjust the infusion rate as needed. The titration process may be repeated until the patient achieves a stable therapeutic range.
It's crucial to follow the specific protocols and guidelines established by the healthcare institution and the healthcare provider. The titration process should be carried out with careful consideration of the individual patient's clinical status and risk factors for bleeding or clotting. Always consult with the healthcare team for guidance in titrating heparin or any other anticoagulant therapy.
Understanding the principles of heparin titration and its clinical applications
Heparin titration is the process of adjusting the dosage of heparin, an anticoagulant medication, to achieve a desired level of anticoagulation. It is a crucial aspect of managing patients at risk of thromboembolic complications, such as deep vein thrombosis (DVT) or pulmonary embolism (PE).
Factors to Consider When Titrating Heparin Drip
Several factors influence heparin titration, including:
Patient Characteristics: Age, weight, renal function, and liver function can affect heparin metabolism and anticoagulant response.
Coagulation Status: Initial coagulation tests, such as activated partial thromboplastin time (aPTT) or anti-Xa concentration levels, provide a baseline for heparin titration.
Treatment Goals: The target anticoagulation level may vary depending on the specific clinical indication and the patient's overall health status.
Initial heparin drip dosing and monitoring strategies
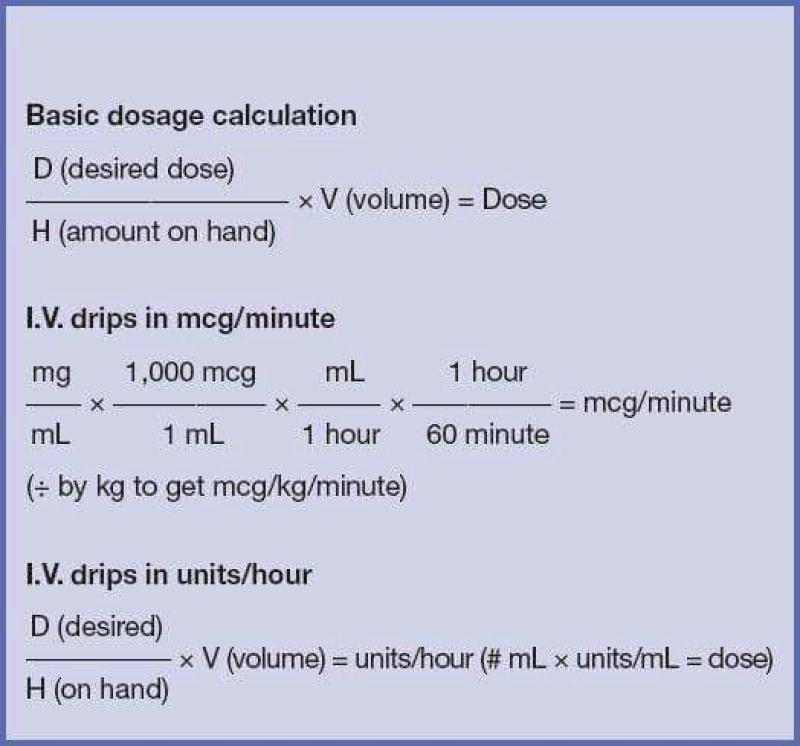
The initial heparin drip rate is typically calculated using weight-based or nomogram-based dosing guidelines. However, individual patient factors and coagulation status should always be considered.
Weight-Based Dosing: This method involves using the patient's weight to determine an initial heparin drip rate.
Nomogram-Based Dosing: Nomograms are charts that consider patient weight, age, and initial coagulation test results to determine an initial heparin drip rate.
Monitoring Coagulation: Regular aPTT or anti-Xa concentration monitoring is essential to assess the patient's anticoagulant response and adjust the heparin drip rate as needed.
Adjusting heparin drip rate based on patient response and laboratory findings
Heparin drip rate adjustments are guided by the patient's clinical response and laboratory findings:
Clinical Response: Signs of excessive anticoagulation, such as bleeding, require heparin drip rate reduction. Conversely, inadequate anticoagulation may necessitate an increase in the heparin drip rate.
Laboratory Findings: aPTT or anti-Xa concentration levels should be maintained within the therapeutic range to achieve optimal anticoagulation.
Weaning and discontinuing heparin drip safely and effectively
Once the patient's condition stabilizes and the risk of thromboembolic complications decreases, heparin weaning can be considered.
Gradual Reduction: Heparin drip rate is gradually reduced over several days to allow the patient's body to adjust to a lower anticoagulant level.
Close Monitoring: Continue monitoring coagulation status and clinical response during weaning to ensure patient safety.
Discontinuation Criteria: Heparin discontinuation is typically considered when the patient's coagulation status has normalized and the risk of thromboembolic complications is low.
Heparin titration is a dynamic process that requires careful consideration of patient factors, coagulation status, and treatment goals. Regular monitoring and individualized adjustments are crucial for achieving optimal anticoagulation and ensuring patient safety.