What are the components of a comprehensive health assessment?
A comprehensive health assessment is a systematic and thorough evaluation of an individual's overall health status. It involves gathering detailed information about the individual's physical, mental, emotional, and social well-being. Healthcare providers, such as physicians, nurses, or nurse practitioners, conduct comprehensive health assessments to develop a complete picture of the patient's health and make informed decisions regarding diagnosis, treatment, and ongoing care. Here are the key components of a comprehensive health assessment:
Health History:
- Gathering information about the patient's medical history, including previous illnesses, surgeries, allergies, and chronic conditions. Family medical history is also considered.
Chief Complaint (CC):
- Identifying the primary reason for the patient's visit or the main health concern that brings them to seek healthcare.
Present Illness (PI):
- A detailed exploration of the patient's current health issues, including the onset of symptoms, their progression, duration, and any factors that worsen or alleviate them.
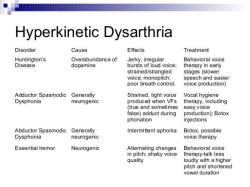
Review of Systems (ROS):
- A systematic inquiry into various body systems (e.g., cardiovascular, respiratory, gastrointestinal) to identify any additional symptoms or issues that may not be part of the chief complaint.
Physical Examination:
- A comprehensive physical examination, including vital signs (e.g., blood pressure, heart rate, temperature), assessment of organ systems, palpation, percussion, and auscultation.
Mental and Emotional Health Assessment:
- Evaluating the patient's mental and emotional well-being, including questions about stress, anxiety, depression, cognitive function, and overall mental health.
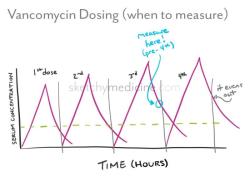
Medication Review:
- Reviewing all current medications, including prescription drugs, over-the-counter medications, and dietary supplements, to assess for potential interactions, side effects, and adherence.
Lifestyle and Health Behaviors:
- Inquiring about the patient's lifestyle choices, including diet, exercise habits, smoking, alcohol and substance use, sexual history, and safety practices.
Functional Assessment:
- Evaluating the patient's ability to perform activities of daily living (ADLs), instrumental activities of daily living (IADLs), mobility, and any limitations in function.
Social and Cultural Factors:
- Considering the patient's social determinants of health, including socioeconomic status, education, living situation, and cultural background, which may influence health and healthcare decisions.
Nutritional Assessment:
- Assessing the patient's nutritional status, dietary habits, and any specific dietary restrictions or nutritional needs.
Risk Assessment:
- Identifying potential health risks and preventive measures, such as exposure to environmental hazards, family history of specific diseases, and lifestyle factors contributing to health issues.
Diagnostic Testing and Laboratory Results:
- Ordering and interpreting diagnostic tests, such as blood tests, imaging studies, and screenings, to aid in diagnosis and treatment planning.
Immunization Status:
- Ensuring that the patient is up-to-date with recommended vaccinations based on age and medical history.
Advance Care Planning:
- Discussing the patient's preferences and decisions regarding end-of-life care, advance directives (e.g., living wills, durable power of attorney for healthcare), and goals of care.
A comprehensive health assessment is a vital tool in healthcare, enabling healthcare providers to develop individualized treatment plans, monitor the patient's progress, and provide patient-centered care. Effective communication and a patient-centered approach are essential during this process to ensure that patients are actively involved in their care and that their concerns, preferences, and goals are considered.