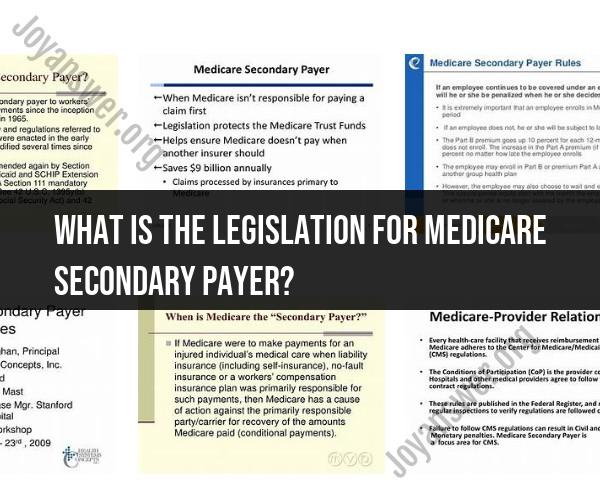
What is the legislation for Medicare Secondary Payer?
The Medicare Secondary Payer (MSP) legislation refers to a series of federal laws and regulations that establish the rules and guidelines for the Medicare program to coordinate benefits with other sources of payment when Medicare is not the primary payer for certain healthcare services. The goal of the MSP legislation is to prevent Medicare from making payments that should rightfully be covered by other insurers or entities. This helps preserve the financial integrity of the Medicare program and ensures appropriate allocation of healthcare costs among responsible parties.
The key pieces of legislation that form the foundation of the Medicare Secondary Payer program include:
1. Medicare as Secondary Payer (MSP) Provisions:Title XVIII, Section 1862(b) of the Social Security Act (42 U.S.C. 1395y(b)) contains the MSP provisions. These provisions establish the framework for Medicare to serve as the secondary payer in situations where other sources of payment are available, such as private health insurance, workers' compensation, liability insurance, and no-fault insurance.
2. Medicare, Medicaid, and SCHIP Extension Act of 2007 (MMSEA):The MMSEA (Public Law 110-173) introduced significant changes to the MSP program. It requires certain insurers and self-insured entities to report information about settlements, judgments, awards, and payments to the Centers for Medicare & Medicaid Services (CMS). This reporting is designed to improve Medicare's ability to identify situations where it should be the secondary payer.
3. Strengthening Medicare and Repaying Taxpayers (SMART) Act:The SMART Act (Public Law 112-242) was enacted in 2013 and introduced further modifications to the MSP program. It aimed to improve the Medicare Secondary Payer Act's efficiency and effectiveness, particularly regarding the recovery of Medicare conditional payments from liability settlements, judgments, or awards.
4. Medicare Access and CHIP Reauthorization Act of 2015 (MACRA):MACRA (Public Law 114-10) included provisions related to Medicare's recovery of conditional payments. It expanded the use of Medicare Advantage and Prescription Drug Plan data for MSP purposes and provided more effective recovery mechanisms for Medicare conditional payments.
5. Bipartisan Budget Act of 2018:This act included changes to the MSP recovery process, allowing Medicare beneficiaries and their representatives to access certain information and dispute claims related to conditional payments.
These legislative acts, along with associated regulations and guidance, define how Medicare coordinates benefits when it's not the primary payer. They establish reporting requirements, recovery processes, and mechanisms to ensure appropriate payment arrangements. It's important to note that the MSP legislation is complex and may undergo changes over time, so individuals and entities involved in healthcare payment and insurance should stay informed about updates and adjustments to the program.