How to get secondary insurance for Medicare?
Secondary insurance for Medicare, often referred to as "Medigap" or "Medicare Supplement Insurance," is designed to cover costs that Medicare doesn't fully pay for, such as deductibles, copayments, and coinsurance. Here are your options for obtaining secondary insurance for Medicare:
Enroll in a Medigap Policy:
- Medigap policies are private insurance plans that work alongside your Original Medicare (Part A and Part B). These policies are standardized and identified by letters (e.g., Plan F, Plan G, Plan N). To enroll in a Medigap policy, follow these steps:a. Determine your eligibility: You must have Medicare Part A and Part B to be eligible for a Medigap policy.b. Compare Medigap plans: Research the available Medigap plans in your area and compare the benefits and costs.c. Choose a plan: Select the Medigap plan that best meets your needs.d. Contact insurance companies: Reach out to insurance companies that offer Medigap policies in your state. They can provide you with plan details, pricing, and enrollment information.e. Enroll during the Open Enrollment Period: The best time to enroll in a Medigap policy is during your 6-month Open Enrollment Period, which begins the month you turn 65 and are enrolled in Medicare Part B. During this period, insurance companies cannot deny you coverage or charge higher premiums based on your health.
Join a Medicare Advantage Plan:
- Instead of enrolling in a Medigap policy, you can choose a Medicare Advantage plan (Part C). These plans are offered by private insurance companies and often provide additional coverage beyond what Original Medicare offers. Some Medicare Advantage plans include prescription drug coverage (Part D) and may cover dental, vision, and other benefits. If you enroll in a Medicare Advantage plan, it becomes your primary insurance, and you don't need a separate Medigap policy.
Medicaid:
- If you have both Medicare and Medicaid, Medicaid may provide additional coverage, including help with Medicare premiums, copayments, and deductibles. To determine your eligibility for Medicaid, contact your state's Medicaid office.
Employer or Union Coverage:
- If you are still working and have health coverage through your employer or a union, you may have the option to keep that coverage as secondary insurance to Medicare. Check with your employer or union benefits administrator for guidance on how to coordinate your coverage.
Retiree Coverage:
- Some retirees receive health insurance coverage as part of their retirement package. This coverage can serve as secondary insurance to Medicare. If you are eligible for retiree coverage, inquire about the terms and conditions for coordination with Medicare.
Military Health Coverage:
- If you have military health coverage, such as TRICARE or the Veterans Affairs (VA) health benefits, these can supplement Medicare. Coordinate with your military or VA benefits office to understand how your coverage works alongside Medicare.
When considering secondary insurance for Medicare, it's essential to assess your healthcare needs, budget, and the specific coverage offered by different plans or options. Medigap policies are standardized but may have different costs and availability depending on your location. If you're considering a Medicare Advantage plan or other secondary insurance options, carefully review the plan details, including coverage, costs, and provider networks, before enrolling. It's also advisable to consult with a Medicare counselor or insurance expert to ensure you make the right choice based on your unique circumstances.
Getting Secondary Insurance for Medicare Recipients
There are a number of ways for Medicare recipients to get secondary insurance. Here are a few options:
- Employer-sponsored health insurance: If you are still working and have employer-sponsored health insurance, your employer's plan will likely be the primary payer for most of your healthcare costs. Medicare will be the secondary payer.
- Medigap: Medigap, also known as Medicare Supplement Insurance, is a type of private insurance that can help pay for Medicare Part A and Part B copays, coinsurance, and deductibles. Medigap plans can also cover certain services that are not covered by Medicare, such as foreign travel emergency coverage.
- Medicare Advantage plans:Medicare Advantage plans are an alternative to Original Medicare. Medicare Advantage plans are offered by private insurance companies and typically provide broader coverage than Original Medicare. Some Medicare Advantage plans also offer additional benefits, such as prescription drug coverage and dental and vision coverage.
Benefits and Coverage of Secondary Medicare Insurance
The benefits and coverage of secondary Medicare insurance will vary depending on the type of plan you choose. However, most secondary Medicare plans will help pay for some or all of the following costs:
- Copays: Copays are fixed amounts that you pay for certain healthcare services, such as doctor's visits and prescription drugs.
- Coinsurance: Coinsurance is a percentage of the cost of a healthcare service that you pay after meeting your deductible.
- Deductibles: Deductibles are amounts that you must pay out-of-pocket before your insurance starts paying for healthcare services.
Finding and Comparing Secondary Medicare Plans
Once you have decided that you want to get secondary Medicare insurance, you can start comparing plans. There are a number of different ways to compare plans, including:
- Using a Medicare plan finder: The Medicare website has a plan finder tool that can help you compare Medigap plans and Medicare Advantage plans.
- Contacting insurance companies directly: You can also contact insurance companies directly to get information about their Medigap plans and Medicare Advantage plans.
- Working with an insurance broker: An insurance broker can help you compare different plans and find the plan that is right for you.
Application and Enrollment Process for Secondary Insurance
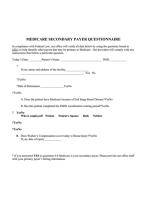
The application and enrollment process for secondary Medicare insurance will vary depending on the type of plan you choose. However, most plans will require you to complete an application and provide some basic information, such as your name, address, and date of birth.
You may also need to provide proof of your Medicare eligibility. Once you have completed the application and provided the required information, your enrollment will be processed and you will receive a welcome packet from your new insurance company.
Financial Considerations and Costs of Secondary Medicare Coverage
The cost of secondary Medicare insurance will vary depending on the type of plan you choose and your age and health. However, most secondary Medicare plans are relatively affordable.
Here are some tips for saving money on secondary Medicare coverage:
- Shop around and compare plans: Compare the premiums, copays, coinsurance, and deductibles of different plans to find the one that is right for you and your budget.
- Consider a Medicare Advantage plan: Medicare Advantage plans often cost less than Medigap plans and offer broader coverage.
- Take advantage of subsidies and discounts: There are a number of subsidies and discounts available to help low-income Medicare recipients afford secondary Medicare coverage.
If you have any questions about secondary Medicare insurance, you can contact Medicare or an insurance broker for assistance.