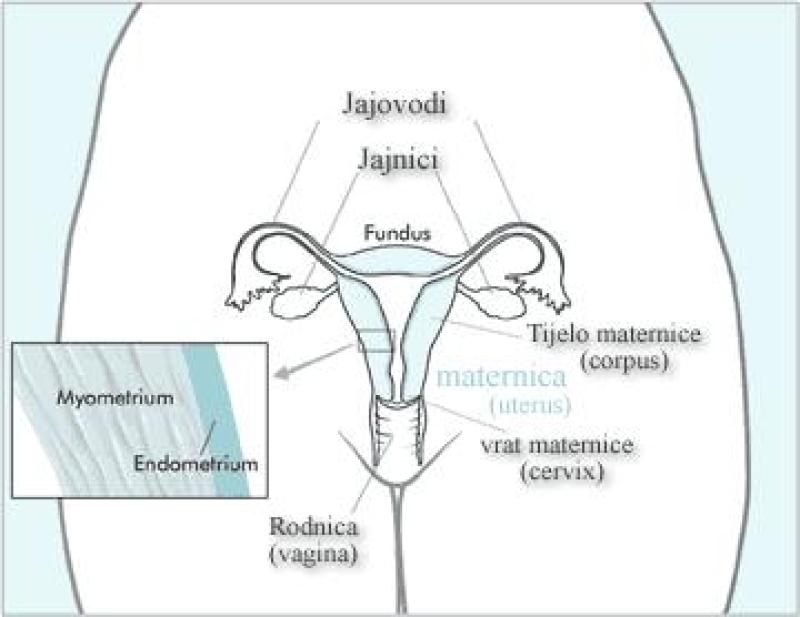
What are the indications for hysterectomy?
Hysterectomy, the surgical removal of the uterus, is performed for various medical reasons. The decision to undergo a hysterectomy is typically based on specific health conditions that significantly impact a person's quality of life or pose serious health risks. Some common indications for hysterectomy include:
Medical Conditions:
Fibroids: Non-cancerous growths in the uterus that can cause pain, heavy menstrual bleeding, and pressure on nearby organs.
Endometriosis: A condition where tissue similar to the lining of the uterus grows outside the uterus, causing severe pain, heavy bleeding, and fertility issues.
Uterine Prolapse: When the uterus descends into the vaginal canal, causing discomfort, urinary incontinence, and pelvic pressure.
Chronic Pelvic Pain: Severe and persistent pain in the pelvic area that significantly affects daily life and does not respond to other treatments.
Abnormal Uterine Bleeding: Excessive, prolonged, or irregular bleeding that doesn't respond to other treatments and affects quality of life.
Cancer: Hysterectomy may be recommended in cases of uterine, cervical, ovarian, or other reproductive cancers.
Adenomyosis: A condition where the tissue that lines the uterus grows into the muscular wall, leading to heavy periods, pain, and swelling of the uterus.
Chronic Pelvic Inflammatory Disease (PID): Severe and recurrent infections of the reproductive organs that can lead to chronic pain and damage to the uterus.
Types of Hysterectomy:
Total Hysterectomy: Removal of the uterus and cervix.
Partial or Supracervical Hysterectomy: Removal of the upper part of the uterus, leaving the cervix intact.
Radical Hysterectomy: In cases of cancer, removal of the uterus, cervix, part of the vagina, and possibly nearby tissues or lymph nodes.
Decision-Making:
The decision to undergo a hysterectomy is a significant one and involves careful consideration by the patient and their healthcare provider. It's essential to discuss the risks, benefits, alternative treatments, and potential impact on fertility and hormonal balance before opting for surgery.
Each case is unique, and the specific indications for a hysterectomy can vary based on individual health conditions, symptoms, and medical history. A thorough evaluation by a healthcare professional is crucial in determining whether a hysterectomy is the most appropriate treatment option.
Addressing Non-Malignant Conditions
Fibroids:
Uterine fibroids are noncancerous tumors that grow in the uterus. They are the most common type of gynecological tumor and affect up to 70% of women by age 50. Most fibroids do not cause symptoms, but some women may experience heavy bleeding, pain, or pressure in the pelvis.
Treatment options for fibroids include:
Observation: For small, asymptomatic fibroids, observation is often the best course of action.
Medication: Medications, such as hormonal birth control or nonsteroidal anti-inflammatory drugs (NSAIDs), can help to manage symptoms of fibroids.
Minimally invasive procedures: Minimally invasive procedures, such as uterine artery embolization (UAE) or myomectomy, can be used to shrink or remove fibroids without removing the uterus.
Hysterectomy: Hysterectomy, which is the removal of the uterus, is sometimes recommended for women with large fibroids that are causing severe symptoms.
Endometriosis:
Endometriosis is a condition in which tissue similar to the lining of the uterus (endometrium) grows outside of the uterus. This tissue can grow on the ovaries, fallopian tubes, bladder, and other organs in the pelvis. Endometriosis can cause pain, infertility, and heavy bleeding.
Treatment options for endometriosis include:
Medication: Medications, such as hormonal birth control or pain medication, can help to manage symptoms of endometriosis.
Surgery: Surgery can be used to remove endometrial tissue that is causing pain or infertility.
Managing Uterine Prolapse and Severe Menorrhagia
Uterine Prolapse:
Uterine prolapse is a condition in which the uterus descends from its normal position in the pelvis. This can happen due to weak pelvic muscles and ligaments. Symptoms of uterine prolapse can include a feeling of heaviness or dragging in the pelvis, pain during intercourse, and urinary incontinence.
Treatment options for uterine prolapse include:
Pelvic floor exercises: Pelvic floor exercises can help to strengthen the muscles that support the uterus.
Pessaries: Pessaries are devices that are inserted into the vagina to help support the uterus.
Surgery: Surgery may be recommended for women with severe uterine prolapse who do not respond to other treatments.
Severe Menorrhagia:
Severe menorrhagia is heavy menstrual bleeding that lasts for more than eight days or causes so much bleeding that it interferes with a woman's daily activities.
Treatment options for severe menorrhagia include:
Hormonal birth control: Hormonal birth control can help to regulate menstrual bleeding.
Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs can help to reduce pain and bleeding during menstruation.
Endometrial ablation: Endometrial ablation is a procedure that destroys the lining of the uterus, reducing menstrual bleeding.
Hysterectomy: Hysterectomy is sometimes recommended for women with severe menorrhagia who do not respond to other treatments.