Does Medicaid pay for medical marijuana?
No, Medicaid does not cover medical marijuana in any U.S. state.
Here’s why:
Federal law: Marijuana is still classified as a Schedule I controlled substance under federal law. Since Medicaid is a federally funded program, it cannot legally reimburse or pay for substances that are federally illegal.
State laws vary: While many states have legalized medical marijuana and issue medical marijuana cards, coverage must still comply with federal regulations—so even in legal states, patients pay out-of-pocket.
What Medicaid may cover (in some states):
FDA-approved cannabis-based medications, such as:
Epidiolex (for certain forms of epilepsy) — may be covered by Medicaid.
Dronabinol (synthetic THC) — sometimes covered.
These medications are different from raw or dispensary-sold marijuana.
Summary:
No, Medicaid does not pay for medical marijuana, even in states where it’s legal. Patients must pay for it themselves. However, FDA-approved cannabinoid medications might be covered.
Medicaid and Medical Marijuana: A Complex Landscape of Coverage
The landscape of medical marijuana in the United States is a patchwork of state-level legalization and federal prohibition, creating significant challenges for patients seeking coverage for cannabis-based treatments.
Does Medicaid Cover Medical Marijuana Expenses?
No, as a general rule, Medicaid does not cover the cost of medical marijuana products or medical marijuana cards.
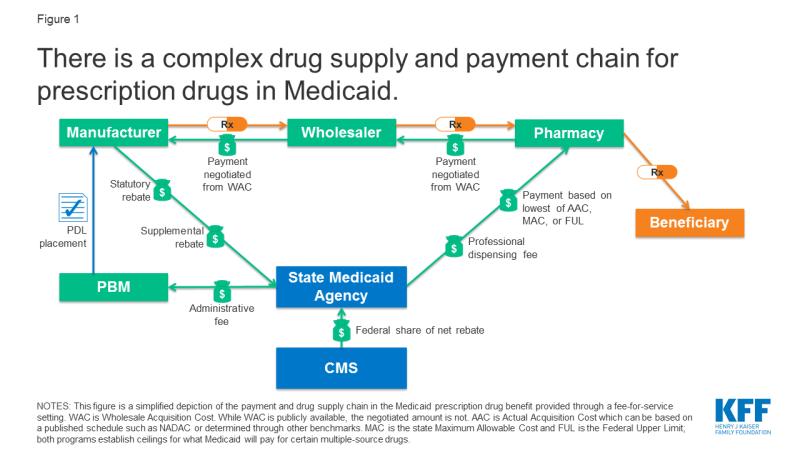
Since Medicaid is a federal-state partnership program, it must adhere to federal laws.
However, there's a nuanced exception: some states allow Medicaid to reimburse for office visits related to the evaluation and certification for medical cannabis.
Why Doesn’t Medicaid Pay for Cannabis Treatments?
The primary reason Medicaid (and Medicare) does not cover cannabis treatments stems directly from its federal illegality.
Federal Classification as Schedule I: As mentioned, the DEA's classification of marijuana as a Schedule I drug is the fundamental barrier.
This status prevents federal programs from recognizing it as a legitimate medicine that can be prescribed or covered. Lack of FDA Approval: For a medication to be covered by federal programs like Medicaid, it generally needs to be approved by the Food and Drug Administration (FDA).
The FDA has not approved whole-plant cannabis for medical use. While some cannabis-derived or synthetic cannabinoid medications have received FDA approval (e.g., dronabinol, nabilone, and Epidiolex), these are distinct pharmaceutical products, not the raw plant material or products sold in state-regulated dispensaries. No Federal Prescription Authority: Doctors cannot federally "prescribe" marijuana; they can only "recommend" its use in states where it's legal.
This distinction is critical for insurance and government program coverage.
Are There Any Exceptions or Pilot Programs?
While direct coverage for medical marijuana products is virtually non-existent under Medicaid, there are a few related areas and considerations:
FDA-Approved Cannabinoid Medications: Medicaid may provide coverage for FDA-approved synthetic or cannabis-derived medications like:
Dronabinol (Marinol, Syndros): A synthetic form of THC used to treat nausea and vomiting in chemotherapy patients and to stimulate appetite in AIDS patients.
Epidiolex: A non-synthetic cannabidiol (CBD) oral solution approved for treating seizures associated with specific rare forms of epilepsy.
These medications are treated like other prescription drugs and are subject to the same formulary rules, prior authorization, and cost-sharing requirements.
Office Visit Reimbursement: As noted, some states, like New York, explicitly clarify that practitioner office visits for medical cannabis evaluation and certification are Medicaid reimbursable services, provided the practitioner participates with Medicaid.
State-Specific Assistance Programs (Not Medicaid Coverage): Some states with medical marijuana programs have established their own assistance programs for low-income patients to help with the cost of medical marijuana cards or, less commonly, the products themselves. These are state-funded initiatives separate from federal Medicaid dollars. For example, Pennsylvania has a Medical Marijuana Assistance Program (MMAP), which may offer some support.
These are not direct Medicaid coverage, but rather complementary state programs.
Can You Get Reimbursed for Medical Marijuana Use?
Direct reimbursement for the purchase of medical marijuana from dispensaries by Medicaid is not possible. As established, federal law prohibits such coverage.
Even for the associated costs, like the medical marijuana card application and renewal fees (which can range from $50 to $200 annually), Medicaid generally does not cover these. The only potential "reimbursement" or coverage related to medical cannabis through Medicaid is for the doctor's visit itself, if that doctor accepts Medicaid for the consultation.
How Do State Laws Impact Medicaid Coverage?
State laws play a crucial role in the legality and accessibility of medical marijuana, but they do not override federal law when it comes to Medicaid coverage.
State Legalization vs. Federal Prohibition: Currently, the vast majority of U.S. states have legalized medical marijuana in some form.
These state laws create the legal framework for patients to access cannabis products within their borders. However, because marijuana remains federally illegal, federal programs like Medicaid cannot recognize or fund these state-legal activities. Indirect Impact: While state laws don't enable direct Medicaid coverage, they can have indirect effects:
Reduced Prescription Drug Use: Studies have suggested that in states with medical marijuana laws, Medicaid enrollees might fill fewer prescriptions for certain conditions (e.g., pain, anxiety), potentially leading to cost savings for the Medicaid program in those areas.
This suggests that patients may be substituting medical marijuana for other prescription drugs. State-Level Assistance: As mentioned, state laws can enable the creation of state-specific financial assistance programs for medical marijuana patients, which operate independently of Medicaid funding.
Defining Qualifying Conditions: State laws define the qualifying medical conditions for which patients can obtain a medical marijuana card, influencing who can even consider cannabis as a treatment option.
In summary, while states have made significant strides in legalizing medical marijuana, the federal stance continues to be the decisive factor preventing Medicaid from covering the costs of cannabis products.