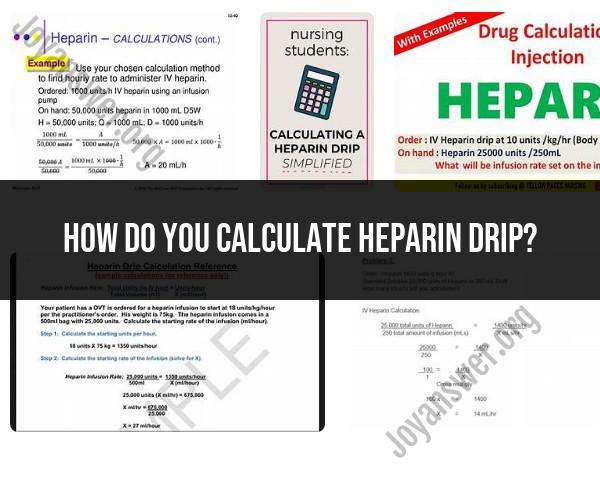
How do you calculate heparin drip?
Calculating a heparin drip involves determining the infusion rate based on the prescribed dosage and the concentration of the heparin solution. Heparin is often administered as a continuous intravenous (IV) infusion, and the rate is usually expressed in units per hour. Here's a step-by-step procedure to calculate a heparin drip:
Step 1: Gather Information
Prescribed Dosage:
- Know the prescribed dosage of heparin. This is typically given in units per kilogram of body weight per hour (e.g., 800 units/hour).
Heparin Concentration:
- Check the concentration of the heparin solution. Common concentrations are 1,000 units/mL or 5,000 units/mL.
Patient's Weight:
- Obtain the patient's weight in kilograms.
Step 2: Determine Total Units Required
- Multiply the prescribed dosage by the patient's weight in kilograms to determine the total units required per hour.
Step 3: Convert Concentration if Needed
- If the heparin concentration is different from the prescribed dosage unit (e.g., if the concentration is 1,000 units/mL but the dosage is given in units/kg/hour), convert the concentration accordingly.
Step 4: Calculate Rate
- Divide the total units required by the heparin concentration to find the rate in milliliters per hour.
Step 5: Set Up Proportions
- If the concentration is in units/mL, set up a proportion to calculate the rate:
Solve for X to find the infusion rate in milliliters per hour.
Step 6: Check the Result
- Verify that the calculated rate is within safe and acceptable ranges. The healthcare provider's order and hospital policies should guide this.
Example:
- Prescribed dosage: 800 units/kg/hour
- Patient's weight: 70 kg
- Heparin concentration: 1,000 units/mL
In this example, the heparin drip rate would be set at 56 mL/hour.
Always ensure that the calculated rate is consistent with the healthcare provider's order and hospital policies. If in doubt or if there are variations in practice at your institution, consult with a pharmacist or another healthcare professional.
Determining Initial Heparin Dose Based on Patient Weight and Coagulation Status
The initial heparin dose is typically determined based on the patient's weight and coagulation status. For unfractionated heparin (UFH), the recommended initial dose is 50 units/kg of body weight administered intravenously (IV) over a 30-minute period. For low molecular weight heparins (LMWHs), the initial dose is typically 100 units/kg of body weight administered subcutaneously (SC) once or twice daily.
The coagulation status of the patient also influences the initial heparin dose. For patients with normal coagulation, the recommended initial dose is sufficient. However, for patients with impaired coagulation, a higher initial dose may be required. Conversely, for patients with heightened bleeding risk, a lower initial dose may be necessary.
Calculating Heparin Drip Rate Based on Desired Antithrombotic Effect
The heparin drip rate is calculated based on the desired antithrombotic effect, which is typically measured by the activated partial thromboplastin time (aPTT). The aPTT is a coagulation test that measures the time it takes for plasma to clot after the addition of activating agents. The target aPTT for most heparin indications is between 1.5 and 2 times the baseline aPTT.
The heparin drip rate is calculated using the following formula:
Drip rate (mL/hr) = (Desired aPTT - Current aPTT) × (Patient weight in kg) × (Constant)
The constant is a value that varies depending on the type of heparin and the desired anticoagulant effect. For UFH, the constant is typically 10. For LMWHs, the constant is typically 4.
Adjusting Heparin Drip Rate Based on Laboratory Monitoring
The heparin drip rate should be adjusted based on laboratory monitoring of the aPTT. The aPTT should be measured 4-6 hours after the initiation of heparin therapy and then every 4-6 hours thereafter until the aPTT is within the desired range. Once the aPTT is stable, the frequency of monitoring can be reduced to once or twice daily.
If the aPTT is below the desired range, the heparin drip rate should be increased. If the aPTT is above the desired range, the heparin drip rate should be decreased. The adjustments should be made in small increments to avoid over- or under-anticoagulation.
In addition to monitoring the aPTT, other coagulation tests, such as the prothrombin time (PT) and antithrombin III (ATIII) level, should also be monitored periodically to ensure adequate anticoagulant control and prevent potential bleeding or thrombosis.