What is the lowest risk strategy for switching between antipsychotics?
Switching between antipsychotic medications should be done under the guidance and supervision of a qualified healthcare provider, such as a psychiatrist, to minimize risks and ensure a smooth transition. The lowest risk strategy for switching between antipsychotics involves careful planning, monitoring, and close communication between the patient and healthcare provider. Here are key steps in a low-risk antipsychotic switch:
Consult with a Healthcare Provider:
- Before making any changes to antipsychotic medications, consult with a qualified healthcare provider, ideally a psychiatrist. Discuss the reasons for the switch, your treatment goals, and any concerns or side effects you've experienced with your current medication.
Assessment and Evaluation:
- Your healthcare provider will conduct a thorough assessment of your current condition and medication history. This assessment helps determine the most appropriate new antipsychotic and the optimal timing for the switch.
Selection of the New Antipsychotic:
- Your healthcare provider will select a new antipsychotic medication based on factors such as your diagnosis, individual response to medications, potential side effects, and your treatment preferences. The choice of the new medication is critical for a successful switch.
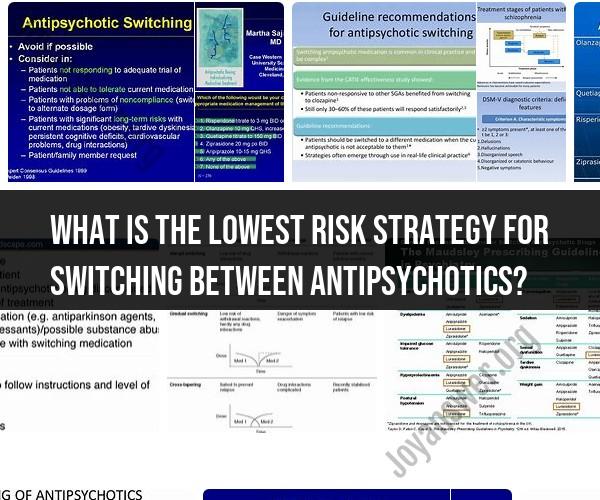
Cross-Titration:
- In most cases, the switch from one antipsychotic to another involves a gradual process called cross-titration or cross-tapering. This means that you will gradually reduce the dose of the current medication while simultaneously increasing the dose of the new medication. This gradual transition minimizes the risk of withdrawal symptoms or exacerbation of symptoms.
Monitoring and Adjustments:
- During the switch, you'll be closely monitored by your healthcare provider. They will assess your symptoms, side effects, and overall well-being. Any adjustments to the dosage or schedule will be made as needed to ensure a smooth transition.
Patient Education:
- Your healthcare provider should educate you about the new medication, including its potential side effects, benefits, and expected outcomes. It's important to have a clear understanding of what to expect during the transition.
Support and Follow-Up:
- Stay in regular contact with your healthcare provider throughout the switch process. If you experience any significant side effects or worsening of symptoms, report them promptly. Your provider can make necessary adjustments to your treatment plan.
Psychosocial Support:
- Consider incorporating psychosocial support into your treatment plan, such as therapy or support groups, to address any psychological or social factors that may affect your response to the new medication.
Medication Adherence:
- Be diligent about taking your medications as prescribed during the switch. Missing doses or altering the prescribed schedule can disrupt the transition process.
Safety Precautions:
- If you experience severe side effects or worsening symptoms, seek immediate medical attention. Have a support system in place, including family members or friends who can assist you during the switch.
Switching between antipsychotic medications can be complex, and the approach should be individualized to your specific needs and circumstances. The goal is to minimize the risk of relapse, withdrawal, or destabilization while optimizing the benefits of the new medication. Always follow your healthcare provider's guidance and maintain open communication throughout the switch process.