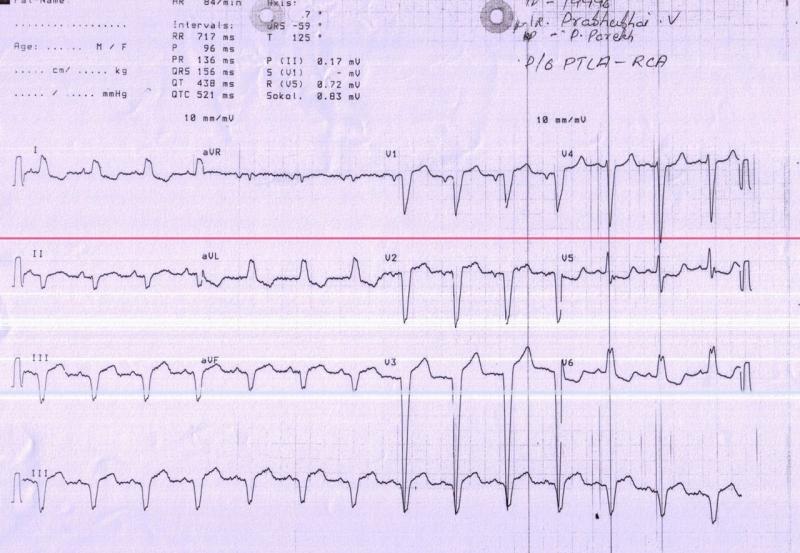
What does inferior infarct on ECG mean?
An "inferior infarct" on an electrocardiogram (ECG or EKG) refers to an area of the heart that has experienced a myocardial infarction (heart attack) in the inferior part of the heart. The term "inferior" in this context typically refers to the lower part of the heart.
The ECG is a diagnostic tool used to record the electrical activity of the heart over a period of time. By analyzing the various waves and complexes on the ECG tracing, healthcare professionals can identify patterns associated with different cardiac conditions, including myocardial infarction.
When an inferior infarct is present on an ECG, it suggests that the blood supply to the inferior part of the heart has been compromised, leading to damage to the heart muscle in that region. The blood supply to the heart is provided by coronary arteries, and if one of these arteries becomes blocked, it can result in a lack of oxygen and nutrients to the affected area, leading to tissue damage (infarction).
Key features on an ECG that may indicate an inferior infarct include:
ST-Segment Elevation:
- Elevation of the ST segment in specific leads on the ECG, often in the inferior leads, such as II, III, and aVF. ST-segment elevation is a common sign of acute myocardial infarction.
T-Wave Changes:
- T-wave changes, including inversion or flattening, may be observed in leads corresponding to the affected area.
Pathological Q-Waves:
- Over time, Q-waves may develop in the affected leads, indicating permanent damage to the heart tissue.
Clinical Correlation:
- The interpretation of an inferior infarct on an ECG should be correlated with the patient's clinical presentation, symptoms, and other diagnostic tests, such as blood tests (cardiac enzymes) and imaging studies (e.g., echocardiogram).
It's important to note that the interpretation of an ECG and the diagnosis of a myocardial infarction require expertise, and healthcare professionals, particularly cardiologists, are trained to analyze these results. Early recognition of myocardial infarction is crucial for prompt intervention and treatment to minimize damage to the heart muscle and improve outcomes. If an inferior infarct is suspected based on an ECG, additional diagnostic tests and medical evaluation are typically conducted to confirm the diagnosis and determine the appropriate course of action.
How is an inferior infarct interpreted on an electrocardiogram (ECG)?
Interpreting an inferior infarct on an electrocardiogram (ECG) requires analyzing specific features:
1. ST Segment Elevation:
- The most significant finding in an inferior infarct is ST segment elevation in the inferior leads (II, III, and aVF).
- The degree of elevation can vary depending on the size and location of the infarct.
- Additionally, ST elevation in lead V1 and V2 may be present, suggesting right ventricular involvement.
2. Reciprocal ST Segment Depression:
- In some cases, reciprocal ST segment depression may be seen in the lateral leads (I, aVL, V5, and V6).
- This occurs because the electrical activity is shifted away from the infarcted area, creating a "mirror image" effect.
3. Q Waves:
- Pathological Q waves (wide and deep) may be present in the inferior leads, indicating necrotic tissue.
- However, Q waves are not always present, especially in small infarcts.
4. T Wave Inversion:
- T wave inversion is a common finding in the inferior leads following an infarct.
- This reflects the ongoing process of injury and healing in the heart muscle.
5. Other Considerations:
- The presence of other ECG abnormalities, such as arrhythmias or conduction disturbances, may further support the diagnosis of an inferior infarct.
- Serial ECGs over time can track the evolution of the infarct and help assess the patient's condition.
Here are some additional points to remember:
- The specific criteria for diagnosing an inferior infarct can vary depending on the guideline used.
- Interpretation of an ECG should always be done in conjunction with other clinical information, such as the patient's symptoms and medical history.
- A cardiologist or other qualified healthcare professional should interpret an ECG and provide a diagnosis.
Here are some helpful resources for further information:
- ECG Library: https://litfl.com/inferior-stemi-ecg-library/
- Mayo Clinic: https://www.ncbi.nlm.nih.gov/books/NBK537076/
- American Heart Association: https://www.heart.org/en/health-topics/heart-attack
By carefully analyzing the ECG features and considering the clinical context, healthcare professionals can accurately interpret an inferior infarct and provide appropriate treatment for the patient.