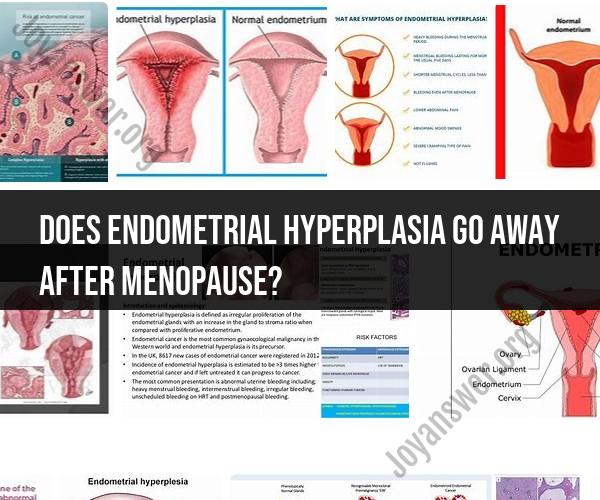
Does endometrial hyperplasia go away after menopause?
Endometrial hyperplasia is the abnormal thickening of the endometrium, the inner lining of the uterus, due to an excess of estrogen relative to progesterone in the body. It is more commonly associated with premenopausal and perimenopausal women, but it can occur in postmenopausal women as well. The course of endometrial hyperplasia in postmenopausal women can vary:
Regression after Menopause: In some cases, endometrial hyperplasia may regress or resolve on its own after menopause. This is because the hormonal changes associated with menopause result in decreased estrogen levels, which can lead to a thinning of the endometrial lining. As a result, the excess estrogen that contributed to hyperplasia diminishes, and the condition may improve.
Persistence: However, endometrial hyperplasia may persist in some postmenopausal women, particularly if it is already at an advanced stage or if other factors, such as obesity or certain medical conditions, are contributing to the hormonal imbalance. In these cases, the condition may not resolve spontaneously.
Increased Risk: Postmenopausal women with endometrial hyperplasia are at an increased risk of developing endometrial cancer, especially if the hyperplasia is of the atypical type. Therefore, any postmenopausal bleeding or abnormal vaginal bleeding should be promptly evaluated by a healthcare provider to rule out cancer and determine the cause.
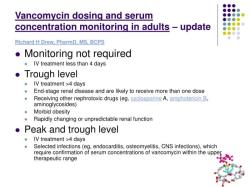
Medical Management: Depending on the type and severity of endometrial hyperplasia in postmenopausal women, healthcare providers may recommend medical management. This can include hormone therapy (progestin therapy) to balance estrogen and progesterone levels and thin the endometrial lining.
Surgical Intervention: In cases of severe or atypical endometrial hyperplasia that do not respond to medical treatment or when cancer is suspected, surgical interventions such as dilation and curettage (D&C) or hysteroscopy with biopsy may be performed to remove the abnormal tissue or to obtain a definitive diagnosis.
It is essential for postmenopausal women who experience abnormal bleeding, spotting, or any concerning gynecological symptoms to seek prompt medical evaluation. Postmenopausal bleeding is not considered normal and should be thoroughly investigated to rule out serious underlying conditions, including endometrial hyperplasia and endometrial cancer.
Regular gynecological check-ups and screenings are also important for postmenopausal women to monitor the health of the endometrium and address any potential issues early on.