What is the definition of blood typing?
Blood typing refers to the process of identifying and categorizing the specific type of blood a person has based on the presence or absence of certain antigens on the surface of red blood cells. The most common blood typing system is the ABO system, which classifies blood into four main groups: A, B, AB, and O. Another important factor in blood typing is the Rh factor, which categorizes blood as Rh-positive or Rh-negative.
Key Components of Blood Typing:
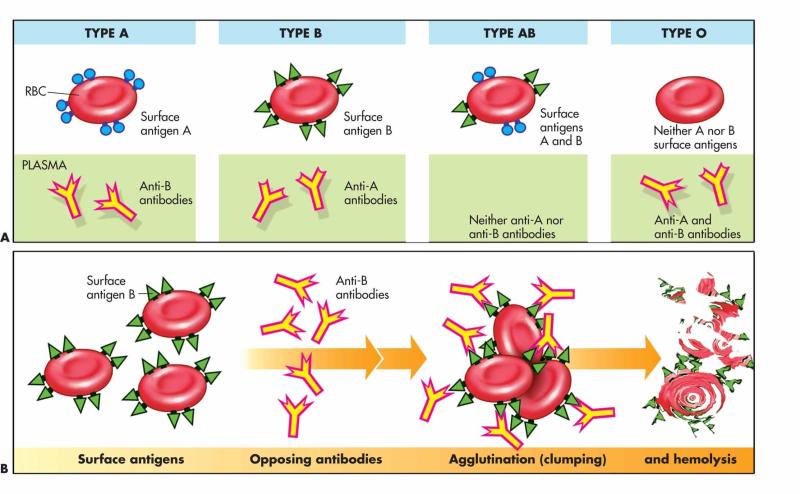
ABO Blood Group System:
- Group A: Individuals with blood type A have A antigens on the surface of their red blood cells and anti-B antibodies in their plasma.
- Group B: Individuals with blood type B have B antigens on the surface of their red blood cells and anti-A antibodies in their plasma.
- Group AB: Individuals with blood type AB have both A and B antigens on the surface of their red blood cells but no anti-A or anti-B antibodies in their plasma.
- Group O: Individuals with blood type O have no A or B antigens on the surface of their red blood cells but have both anti-A and anti-B antibodies in their plasma.
Rh Factor:
- Rh-Positive (Rh+): If a person's red blood cells have the Rh antigen, they are Rh-positive.
- Rh-Negative (Rh-): If a person's red blood cells lack the Rh antigen, they are Rh-negative.
Blood Typing Process:
Blood Sample Collection:
- A small sample of blood is collected from the individual through a vein in the arm.
Testing for ABO and Rh:
- The blood sample is mixed with antibodies specific to the A, B, and Rh antigens. The reactions determine the blood type.
Interpreting Results:
- The presence or absence of agglutination (clumping) in response to the antibodies helps identify the blood type.
Blood Transfusions and Compatibility:
- Knowing a person's blood type is crucial for blood transfusions. Incompatible blood transfusions can lead to a serious and potentially life-threatening reaction.
- Compatibility is determined based on the ABO and Rh types. For example, individuals with blood type A can generally receive blood from donors with blood type A or O, and Rh-positive individuals can receive blood from Rh-positive or Rh-negative donors.
Blood typing is an essential component of blood banking, medical procedures, and emergency medical care to ensure the safe and effective transfusion of blood and blood products.
Understanding the concept of blood types and their significance in blood transfusion and compatibility
Blood types are a crucial aspect of human biology, playing a vital role in blood transfusion and determining compatibility between individuals. The concept of blood types revolves around the presence or absence of specific antigens on the surface of red blood cells (RBCs). These antigens are proteins that act as markers, triggering an immune response if they are recognized as foreign by the recipient's body.
The ABO blood group system and its role in determining blood compatibility
The ABO blood group system is the most widely recognized and important classification system for blood types. It categorizes individuals into four main blood groups: A, B, AB, and O, based on the presence or absence of two antigens, A and B, on RBCs.
Type A: Individuals with type A blood have A antigens on their RBCs but lack B antigens.
Type B: Individuals with type B blood have B antigens on their RBCs but lack A antigens.
Type AB: Individuals with type AB blood possess both A and B antigens on their RBCs.
Type O: Individuals with type O blood have neither A nor B antigens on their RBCs.
The Rh factor and its impact on blood typing and potential complications
In addition to the ABO system, the Rh factor is another important consideration in blood typing. Individuals are either Rh-positive (Rh+) if they have the Rh antigen on their RBCs or Rh-negative (Rh-) if they lack it. The Rh factor can cause complications during pregnancy if an Rh-negative mother carries an Rh-positive fetus. This is because the mother's body may produce antibodies against the Rh antigen on the fetus's RBCs, potentially leading to hemolytic disease of the newborn (HDN).
The importance of blood typing in preventing transfusion reactions and ensuring patient safety
Blood typing is essential for preventing transfusion reactions, which can occur if a recipient receives blood incompatible with their blood type. Transfusion reactions can range from mild symptoms like fever and chills to severe complications like hemolysis, kidney failure, and even death. Proper blood typing ensures that individuals receive compatible blood, minimizing the risk of these adverse reactions and safeguarding patient safety.
Advancements in blood typing technology and their impact on medical diagnostics
Technological advancements have significantly improved blood typing accuracy and efficiency, further enhancing medical diagnostics. These advancements include:
Molecular typing: This technique identifies specific DNA sequences associated with blood groups, providing more precise and reliable typing.
Automated blood typing systems: These systems automate the blood typing process, reducing human error and increasing throughput.
Gel electrophoresis: This method separates RBCs based on their electrical charge, facilitating more accurate identification of blood groups.
These advancements have strengthened the role of blood typing in transfusion medicine, contributing to safer and more effective blood transfusions for patients worldwide.