How to answer medical ethics scenarios?
Approaching medical ethics scenarios involves considering ethical principles, applying relevant guidelines, and using a systematic approach to analyze and respond to the situation. Here's a general guide on how to answer medical ethics scenarios:
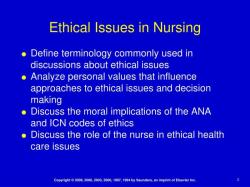
Identify the Ethical Issues:
- Clearly identify the key ethical issues presented in the scenario. This might include considerations related to autonomy, beneficence, non-maleficence, justice, and other ethical principles.
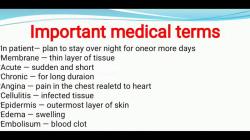
Gather Information:
- Ensure that you have all the necessary information about the patient, the medical condition, and the context. Consider the cultural, social, and legal aspects that may be relevant.
Understand Stakeholders:
- Identify the stakeholders involved, including the patient, healthcare professionals, family members, and others. Consider their perspectives, interests, and potential conflicts.
Apply Ethical Principles:
- Analyze the scenario in light of ethical principles. Consider how each principle might guide or conflict with potential courses of action. For example:
- Autonomy: Respect the patient's right to make decisions.
- Beneficence: Promote the well-being of the patient.
- Non-maleficence: Do no harm to the patient.
- Justice: Distribute resources and benefits fairly.
- Analyze the scenario in light of ethical principles. Consider how each principle might guide or conflict with potential courses of action. For example:
Consider Legal and Institutional Guidelines:
- Be aware of relevant laws, regulations, and institutional policies that may apply to the situation. These may provide guidance on issues such as informed consent, confidentiality, and end-of-life care.
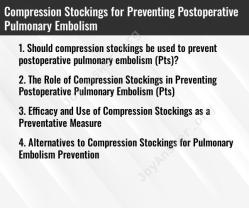
Explore Alternatives:
- Identify and evaluate different courses of action. Consider the potential benefits and harms of each alternative. Think about long-term consequences and the impact on all stakeholders.
Consult Colleagues and Experts:
- Discuss the scenario with colleagues, supervisors, or ethics committees if possible. Seek input from individuals with expertise in medical ethics to gain different perspectives.
Reflect on Personal Values:
- Reflect on your own values and biases. Consider how they might influence your perception of the ethical issues and your proposed solutions. Be open to recognizing and addressing any potential conflicts.
Make a Decision:
- Based on your analysis, make a decision that is ethically justifiable and aligned with the principles of medical ethics. Clearly articulate the reasons behind your decision.
Communicate Effectively:
- Communicate your decision and rationale to relevant stakeholders, ensuring transparency and clarity. Address concerns, answer questions, and involve the patient in decision-making whenever possible.
Review and Reflect:
- After implementing the decision, reflect on the outcomes and whether the chosen course of action achieved the desired ethical goals. Use the experience to inform future decision-making.
Remember that medical ethics scenarios are often complex and may not have a clear-cut solution. The goal is to make well-reasoned decisions that uphold ethical principles and prioritize the well-being of the patient while considering the broader context. Continuous reflection and learning are essential for healthcare professionals engaged in ethical decision-making.
What are the key considerations in resolving medical ethics scenarios?
Resolving medical ethics scenarios can be complex and nuanced, often requiring careful consideration of various factors. Here are some key considerations to guide your approach:
1. Core ethical principles:
- Autonomy: Respecting the patient's right to self-determination and informed decision-making, even if their choices differ from yours.
- Beneficence: Acting in the best interest of the patient to promote their well-being and minimize harm.
- Non-maleficence: Avoiding causing harm to the patient, including physical, emotional, and psychological harm.
- Justice: Ensuring fair and equitable distribution of healthcare resources and treatment options.
2. Contextual factors:
- Patient's values and preferences: Understanding the patient's cultural background, religious beliefs, and personal values can significantly influence their decisions.
- Medical situation: Consider the specific medical diagnosis, prognosis, and treatment options available, along with their risks and benefits.
- Legal and regulatory considerations: Ensure your decisions comply with relevant laws, professional codes of ethics, and institutional policies.
3. Communication and collaboration:
- Open and honest communication: Clearly communicate all relevant information to the patient in a way they can understand, ensuring informed consent.
- Multidisciplinary collaboration: Seek input from relevant healthcare professionals, ethical committees, or legal counsel when needed.
- Family involvement: Respect the role of family members in decision-making when appropriate, considering cultural practices and patient autonomy.
4. Decision-making framework:
- Gather information: Thoroughly assess the situation, gathering all relevant medical, legal, and ethical information.
- Identify conflicting values: Analyze the potential conflicts between competing ethical principles and values at play.
- Consider options and consequences: Weigh the potential benefits and harms of different courses of action.
- Seek ethical guidance: Utilize available resources such as ethics committees, consultants, or professional organizations for additional support.
- Document your decision: Clearly document your reasoning and justification for the chosen course of action.
5. Ongoing considerations:
- Respect for dissent: Accept the patient's right to disagree with your recommendations, even if you believe a different course of action is in their best interest.
- Flexibility and adaptation: Be willing to adapt your approach as new information emerges or the situation evolves.
- Seeking support: Remember to prioritize your own well-being and seek support from colleagues or mental health professionals if needed.
Remember, there are rarely "easy" answers in medical ethics scenarios. However, by using these key considerations as a guide, you can approach these situations with a thoughtful and ethical mindset, striving to provide the best possible care for your patients while respecting their autonomy and well-being.