What are the basic ethical principles for health care?
Basic Ethical Principles for Health Care
1. Autonomy (Respect for the Patient’s Choices)
Patients have the right to make their own health care decisions.
Providers must respect informed consent and allow patients to accept or refuse treatment.
Example: A patient can refuse a blood transfusion based on religious beliefs.
2. Beneficence (Do Good)
Health professionals must act in the best interest of the patient.
Care should aim to improve health, promote well-being, and prevent harm.
Example: Recommending vaccinations to prevent illness.
3. Nonmaleficence (Do No Harm)
Avoid causing unnecessary harm or suffering.
“First, do no harm” (primum non nocere).
Example: Weighing the risks vs. benefits of surgery before proceeding.
4. Justice (Fairness and Equality)
Patients should be treated fairly, without discrimination.
Resources should be distributed equitably, especially in public health.
Example: Providing equal access to emergency care regardless of ability to pay.
5. Confidentiality
Patient information must be kept private and shared only with proper consent or when legally required.
Builds trust between patients and providers.
Example: Following HIPAA regulations in the U.S.
6. Veracity (Truthfulness)
Health care providers should be honest with patients.
Includes full disclosure about diagnosis, treatment options, and risks.
Example: A doctor clearly explaining potential side effects of medication.
7. Fidelity (Loyalty and Keeping Promises)
Providers must honor commitments to patients and maintain professional integrity.
Builds strong patient-provider relationships.
Example: Following through on treatment plans and respecting patient trust.
Summary Table
| Principle | Meaning | Example |
|---|---|---|
| Autonomy | Respect patient decisions | Refusing treatment |
| Beneficence | Promote good and well-being | Giving preventive care |
| Nonmaleficence | Do no harm | Avoiding risky, unnecessary procedures |
| Justice | Fairness and equality | Equal ER access |
| Confidentiality | Protect patient privacy | HIPAA compliance |
| Veracity | Be truthful | Explaining risks honestly |
| Fidelity | Be loyal and keep promises | Following treatment commitments |
Together, these principles form the foundation of medical ethics and are applied daily in clinical decision-making.
Core Ethical Principles in Health Care
The foundation of health care ethics rests on four key principles:
Autonomy: This principle upholds a patient's right to make their own decisions about their medical care. It requires that health care professionals respect a patient's wishes, even if they disagree with them, as long as the patient is mentally competent.
Beneficence: This is the duty to do good for the patient. It means acting in the patient's best interest, promoting their well-being, and providing care that is beneficial to them.
Non-maleficence: The principle of "do no harm." It requires health care providers to avoid causing harm to patients. This includes not only direct harm but also avoiding risks or side effects that are not justified by the potential benefits of the treatment.
Justice: This principle refers to the fair and equitable distribution of health care resources. It means that all patients should be treated justly and fairly, regardless of their socioeconomic status, race, or other characteristics.
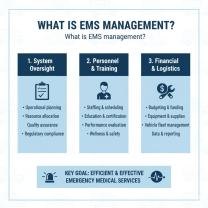
How Ethics Guide Clinical Decision-Making
Ethical principles provide a framework for health care professionals to navigate complex situations. When a clinician makes a decision, they must consider all four principles. For example, when recommending a treatment, a doctor must weigh the potential benefits (beneficence) against the risks (non-maleficence). They must also ensure the patient fully understands the information and makes their own choice (autonomy), and that the decision is fair and just in the broader context (justice). These principles are not always in perfect harmony, which leads to ethical dilemmas.
Examples of Ethical Dilemmas in Health Care
Ethical dilemmas arise when two or more of the core principles conflict. Common examples include:
End-of-Life Care: A patient with a terminal illness may request to stop life-sustaining treatment (autonomy), but the medical team may feel obligated to continue treatment to preserve life (beneficence).
Resource Allocation: During a crisis like a pandemic, doctors may face difficult decisions about who receives a limited number of ventilators. This is a classic conflict between justice (fair distribution) and beneficence (providing care to the most patients).
Patient Confidentiality: A doctor learns that a patient has a condition that could put others at risk. The doctor must balance the patient's right to privacy (autonomy and confidentiality) against the duty to protect others (beneficence).
Importance of Patient Confidentiality
Patient confidentiality is a cornerstone of the doctor-patient relationship and is closely tied to the principle of autonomy. Patients must trust that their personal health information will be kept private. This trust encourages them to be honest with their health care providers, leading to more accurate diagnoses and effective treatment. The Health Insurance Portability and Accountability Act (HIPAA) is a U.S. law that provides strict guidelines for protecting patient information, reinforcing this ethical principle with legal requirements.
Maintaining Professional Integrity in Medical Practice
Professional integrity involves upholding moral and ethical standards in all aspects of medical practice. This includes:
Honesty: Being truthful with patients, colleagues, and the public. This means disclosing medical errors and being transparent about treatment options.
Accountability: Taking responsibility for one's actions and decisions, and being accountable to patients and the profession.
Continuous Learning: Staying up-to-date with medical advancements to ensure that the care provided is based on the best available evidence.
Respect: Treating all patients, colleagues, and staff with respect, regardless of their background or beliefs.
Maintaining professional integrity is not only a personal responsibility but also crucial for maintaining the public's trust in the health care system.